Ratification Date: 21/05/2024
Next Review Date: 31/05/2025
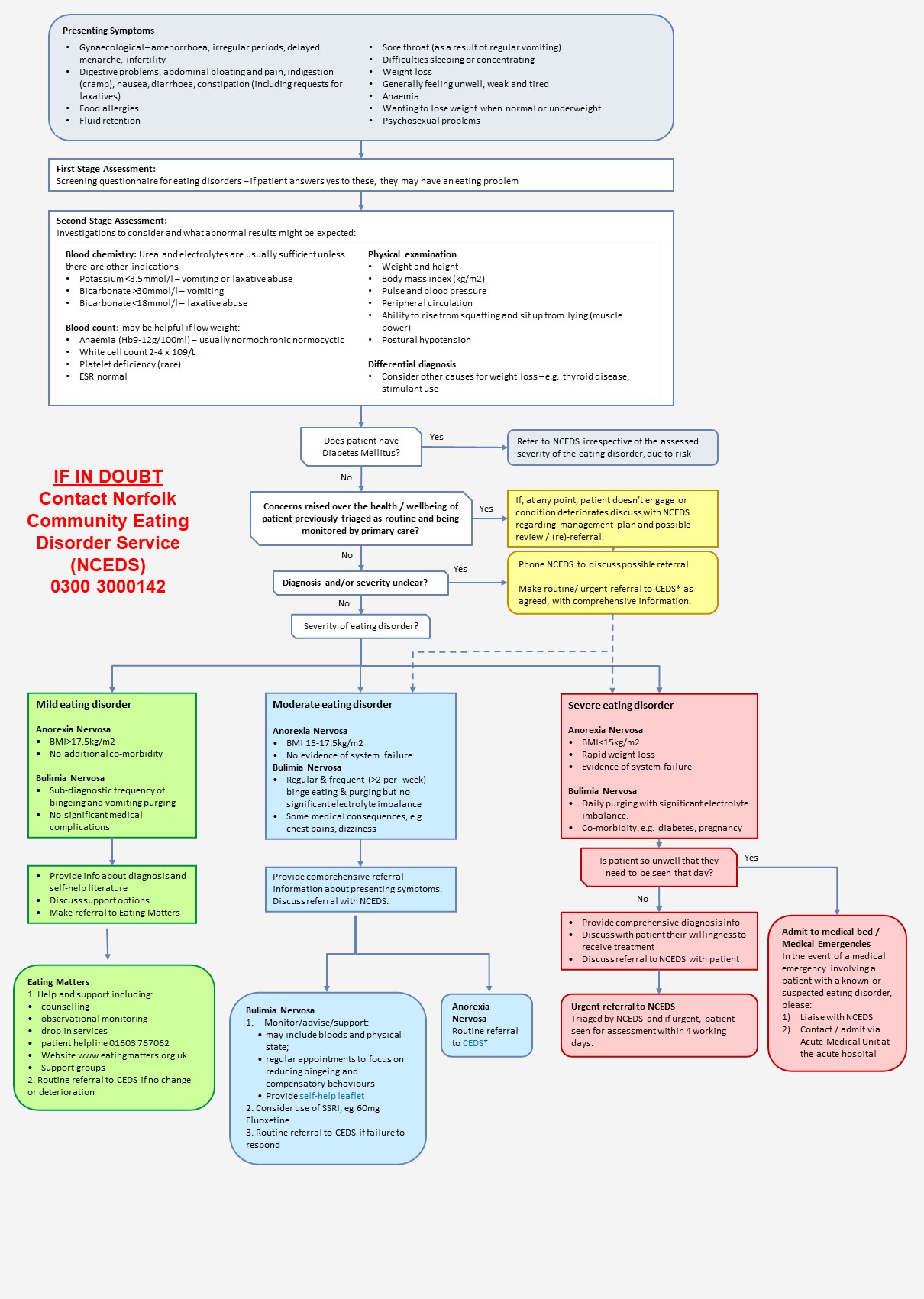
Eating Disorders Care Pathway and Guidance – 18 yrs and over (Norfolk & Waveney)
Eating disorders covered by this pathway/guidance include: anorexia nervosa (AN), bulimia nervosa (BN), and atypical eating disorders in people aged over 18
Diagnostic criteria: Anorexia Nervosa (AN)
- Refusal to maintain body weight over a minimum normal weight for age and height (ie, weight loss leading to body weight 15% below that expected).
- Intense fear of gaining weight or becoming fat even though underweight.
- Disturbance in the way in which their body weight, size or shape is experienced, undue influence of body shape and weight on self-evaluation, or denial of the seriousness of low body weight.
- Amenorrhoea – ie, the absence of at least three consecutive menstrual cycles.
Diagnostic criteria: Bulimia Nervosa (BN)
- Recurrent episodes of binge eating. An episode of binge eating is characterised by both of the following:
- Eating in a discrete period of time (eg, any two-hour period), an amount of food that is definitely larger than most people would eat during a similar period of time in similar circumstances; and
- A sense of lack of control overeating during the episode (eg, feeling that they cannot stop eating or control what or how much they are eating).
- Recurrent inappropriate compensatory behaviour to prevent weight gain such as self-induced vomiting, use of laxatives, diuretics or other medications, fasting or excessive exercise.
- Self evaluation is unduly influenced by body shape and weight.
- The disturbance does not occur exclusively during periods of anorexia nervosa.
Diagnostic criteria: Binge Eating Disorder (BED)
- When people engage in three or more of the following food related behaviours:
- Eating until they feel uncomfortably full
- Eating large amounts of food when they are not physically hungry
- Eating more rapidly than normal
- Eating alone due to embarrassment
- Feeling disgusted, low or guilty after overeating
The binging is not linked to inappropriate compensatory behaviours such as purging or over-exercising
Screening Questions for Eating Disorder
If patients answer yes to the following questions, they may have an eating problem:
- Do you always want to eat less than other people in the family (or your friends)?
- Do you have an intense interest in food and want to cook for others (most dieters want to stay away from food)
- Are you always counting calories?
- Are you worried about the shape of your body or your weight?
- Do you prefer to eat alone?
- Do you like to do a lot of exercise, more than your friends?
- Do you try to disguise your shape by wearing bulky clothes?
Other questions to ask:
- What do you eat in an average day?
- When was your last period?
- Do you ever vomit, use laxatives or diuretics? If so, how much and when?
- Do you ever binge? How often and what do you eat?
- Have you noticed any weakness in your muscles? What about climbing the stairs?
- What is your sleep like?
- Have you fainted or had dizzy spells?
How common are eating disorders?
At any one time, an average GP list of approximately 2000 patients is likely to include:
- 1-2 patients with full anorexia nervosa
- 18 patients with full bulimia nervosa
- 38 patients with atypical eating disorders
- 5-10% of adolescent girls using weight reduction techniques, other than dieting (ie, vomiting, laxative and diuretic abuse, excessive exercising)
Communications from NCEDS to GPs
- All patients attending NCEDS will be assessed and receive a copy of their Keeping Safe plan. A copy of the assessment outcome / Keeping Safe plan will be sent to the patient and their GP.
- The GP and any other professionals involved will be kept informed of the patient’s progress/changes in the care plan.
- Patients discharged from the NCEDS will be given a written relapse prevention plan at discharge as part of their end of therapy letter.
Ongoing monitoring in Primary Care
All patients
Whilst under the care of NCEDS, some patients (particularly those with associated medical risks, e.g. severe anorexia nervosa and rarely severe bulimia nervosa) will require ongoing monitoring from primary care. Details of any recommended tests and monitoring periods will be outlined in each patient’s assessment outcome / care plan. However, this may include:
- U & E, FBC, LFT, glucose, mg, phosphate, calcium, muscle CK,
- ECG
- Weight
- Blood pressure (sitting and standing)
- Temperature
- Squat test
Long term patients with enduring anorexia nervosa:
- Annual check-ups should be offered by primary care, to include the tests mentioned above plus a bone dexa scan if chronically amenorrhoeic
- Patients will also be contacted by NCEDS for an annual review to include a discussion about physical aspects of their condition and the invitation to participate in more active treatment if they are motivated to work on change.

